Healthfirst Prior Authorization Form
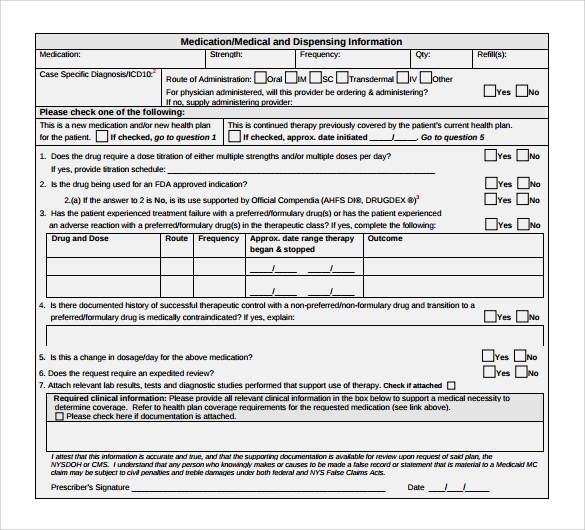
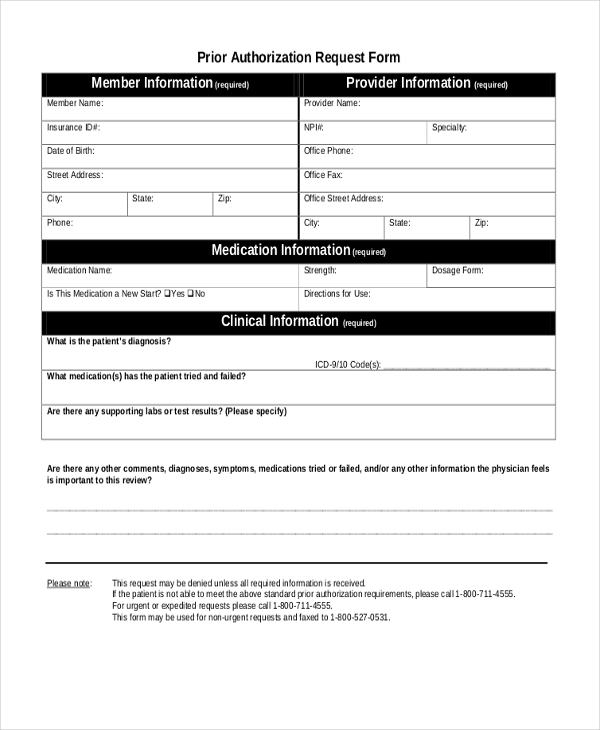
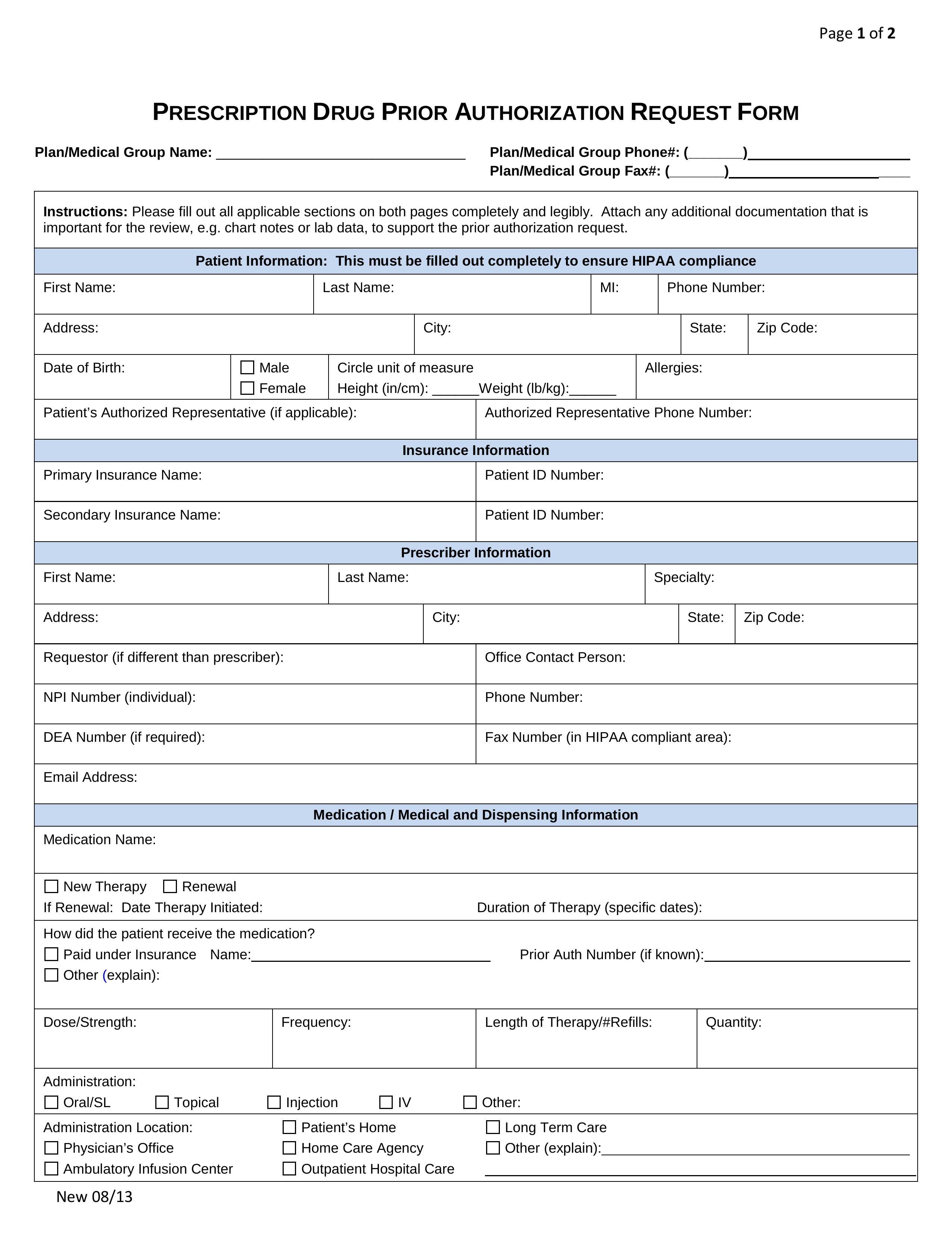
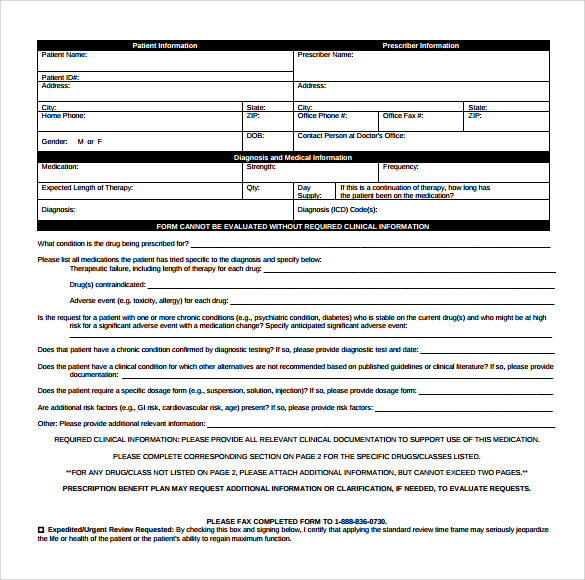
Healthfirst Prior Authorization Form - Web we would like to show you a description here but the site won’t allow us. Web 2022 provider prior authorization form (small and large group commercial plans) provider prior authorization form (medicare and individual plans) provider authorization intake form provider request for medicare prescription drug coverage determination provider request for prescription drug coverage redetermination prescription claim. You must create a user account. To submit authorization check status ; Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Enrollment in health first health plans depends on contract renewal. For the services listed below, the process. Health first health plans is an hmo plan with a medicare contract. Additional information we should consider Web prior authorization submission and status:
Enrollment in health first health plans depends on contract renewal. Additional information we should consider Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. To submit authorization check status ; Health first commercial plans, inc. Covermymeds is healthfirst prior authorization forms’s preferred method for receiving epa requests. For the services listed below, the process. We use both internal and external resources in the authorization process. Request authorization or check status; Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information.
Covermymeds is healthfirst prior authorization forms’s preferred method for receiving epa requests. Web provider prior authorization form provider prior authorization form fax medical authorization requests to: You must create a user account. Web we would like to show you a description here but the site won’t allow us. Request authorization or check status; To submit authorization check status ; We use both internal and external resources in the authorization process. Web select the appropriate healthfirst form to get started. For the services listed below, the process. Web prior authorization submission and status:
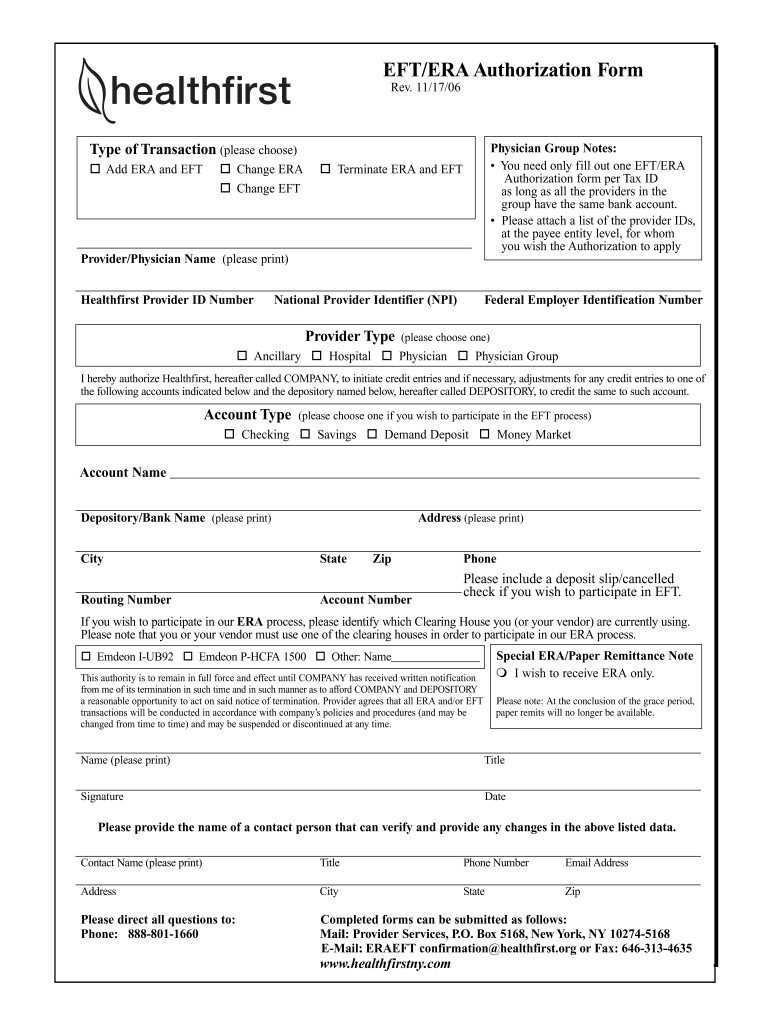
Eft Authorization Form Fill Out and Sign Printable PDF Template signNow
You must create a user account. We use both internal and external resources in the authorization process. Health first commercial plans, inc. Web prior authorization submission and status: An authorized agent is an employee of the prescribing practitioner and has access to the patient's medical records
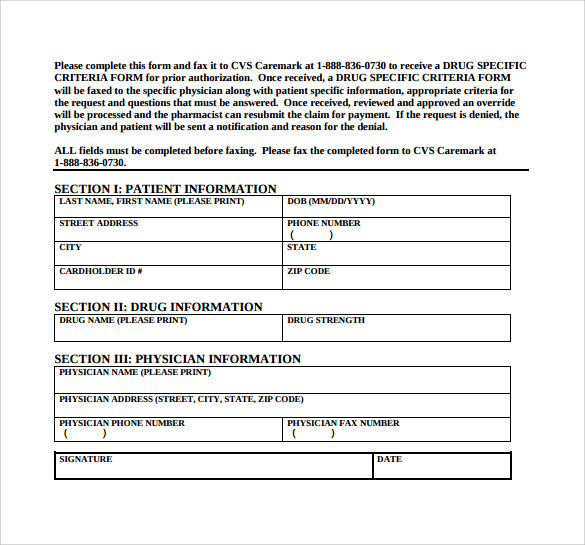
9+ Sample Caremark Prior Authorization Forms Sample Templates
You must create a user account. Request authorization or check status; To submit authorization check status ; Download the phi release form appointment of representative form (aor) Web 2022 provider prior authorization form (small and large group commercial plans) provider prior authorization form (medicare and individual plans) provider authorization intake form provider request for medicare prescription drug coverage determination provider.
Da Form 638 Fillable New Healthfirst Prior Authorization Health
Enrollment in health first health plans depends on contract renewal. Web we would like to show you a description here but the site won’t allow us. Download the phi release form appointment of representative form (aor) Web medical authorization request form fax medical authorization requests to: Health first commercial plans, inc.
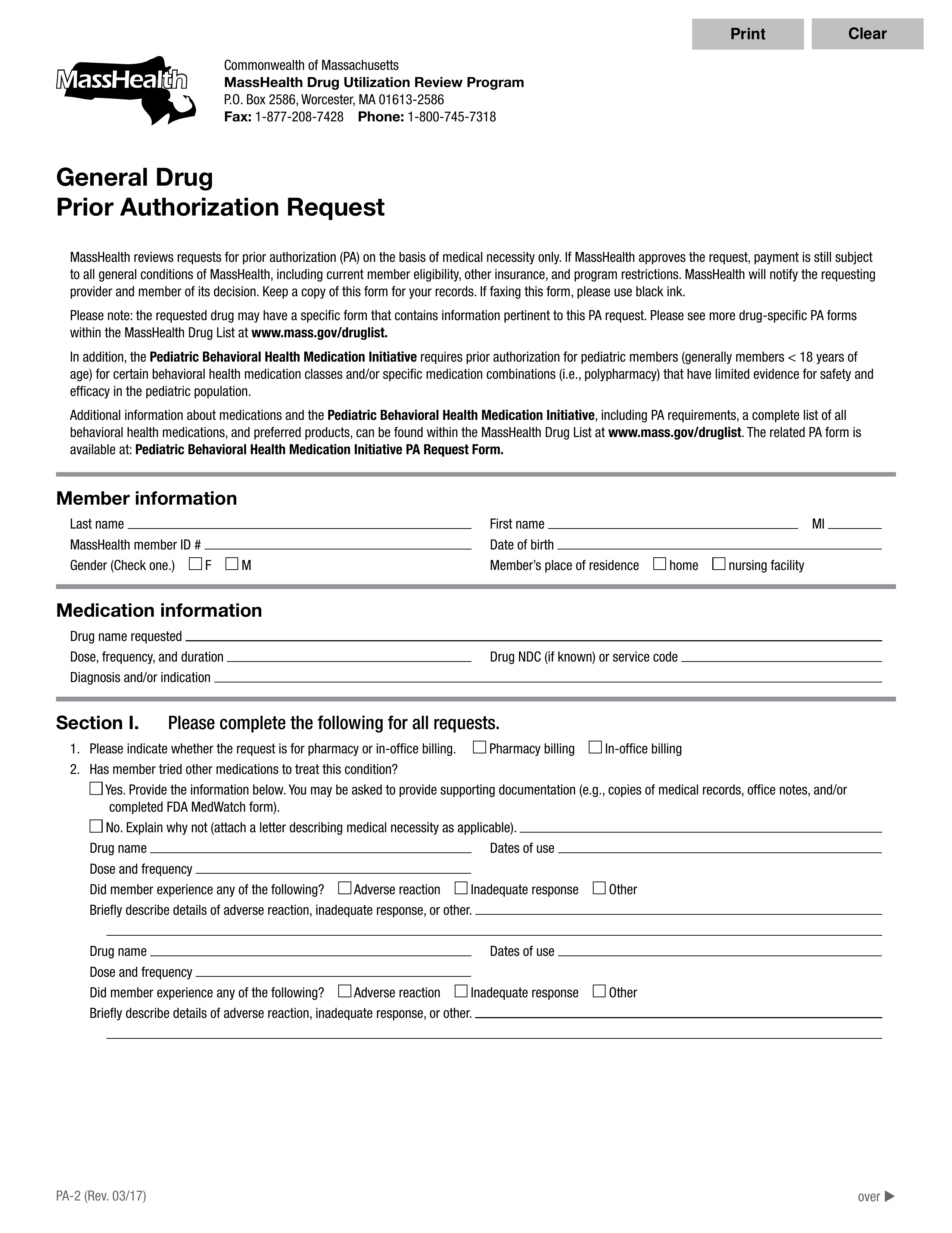
Free MassHealth Prior (Rx) Authorization Form PDF eForms
Web we would like to show you a description here but the site won’t allow us. Your prescriber may use the attached “supporting information for an exception request or prior authorization” to support your request. Web see the current authorization list to determine if prior authorization is required for general categories of services. Web medical authorization request form fax medical.
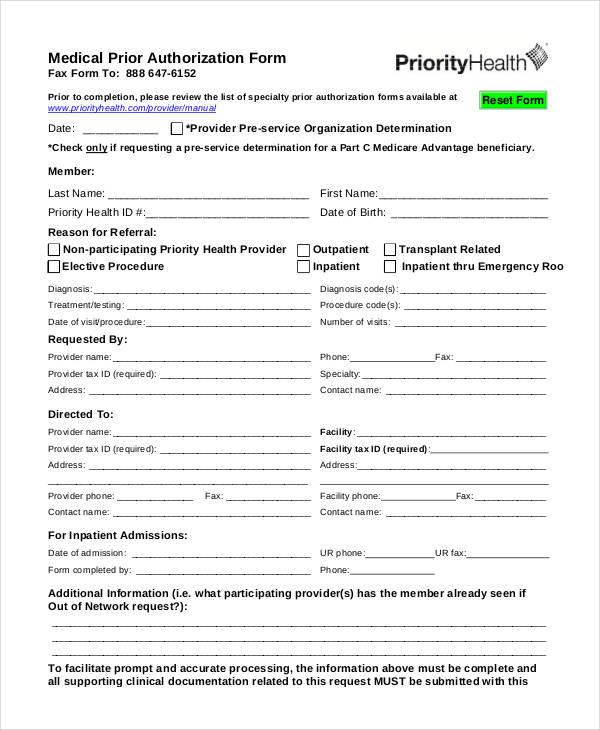
FREE 15+ Medical Authorization Forms in PDF Excel MS Word
Web see the current authorization list to determine if prior authorization is required for general categories of services. Web 2022 provider prior authorization form (small and large group commercial plans) provider prior authorization form (medicare and individual plans) provider authorization intake form provider request for medicare prescription drug coverage determination provider request for prescription drug coverage redetermination prescription claim. An.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Web provider prior authorization form provider prior authorization form fax medical authorization requests to: Web select the appropriate healthfirst form to get started. Enrollment in health first health plans depends on contract renewal. Web this form must be signed by the prescriber but can also be completed by the prescriber or his/her authorized agent. We use both internal and external.
FREE 10+ Sample Medicare Forms in PDF MS Word
Health first health plans is an hmo plan with a medicare contract. Web medical authorization request form fax medical authorization requests to: Web see the current authorization list to determine if prior authorization is required for general categories of services. To begin using our secure site; Enrollment in health first health plans depends on contract renewal.
Free Prior (Rx) Authorization Forms PDF eForms
Enrollment in health first health plans depends on contract renewal. Health first commercial plans, inc. An authorized agent is an employee of the prescribing practitioner and has access to the patient's medical records Download the phi release form appointment of representative form (aor) To submit authorization check status ;
Is Humana And Medicare The Same Health First Plans Parkland
Web see the current authorization list to determine if prior authorization is required for general categories of services. Web select the appropriate healthfirst form to get started. Web medical authorization request form fax medical authorization requests to: We use both internal and external resources in the authorization process. Request authorization or check status;
9+ Sample Caremark Prior Authorization Forms Sample Templates
Additional information we should consider Web provider prior authorization form provider prior authorization form fax medical authorization requests to: Enrollment in health first health plans depends on contract renewal. Request authorization or check status; To begin using our secure site;
You Must Create A User Account.
Web this form must be signed by the prescriber but can also be completed by the prescriber or his/her authorized agent. Health first commercial plans, inc. For the services listed below, the process. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests.
Covermymeds Is Healthfirst Prior Authorization Forms’s Preferred Method For Receiving Epa Requests.
Health first health plans is an hmo plan with a medicare contract. Web see the current authorization list to determine if prior authorization is required for general categories of services. Request authorization or check status; Web provider prior authorization form provider prior authorization form fax medical authorization requests to:
Web Authorization To Release Protected Health Information (Phi) Complete This Form If You Want To Give Someone (Such As A Family Member, Caregiver, Or Another Company) Access To Your Health Or Coverage Information.
Additional information we should consider Enrollment in health first health plans depends on contract renewal. Web select the appropriate healthfirst form to get started. To begin using our secure site;
Web 2022 Provider Prior Authorization Form (Small And Large Group Commercial Plans) Provider Prior Authorization Form (Medicare And Individual Plans) Provider Authorization Intake Form Provider Request For Medicare Prescription Drug Coverage Determination Provider Request For Prescription Drug Coverage Redetermination Prescription Claim.
We use both internal and external resources in the authorization process. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web we would like to show you a description here but the site won’t allow us. Web prior authorization submission and status: